BlueCross BlueShield Nebraska Reconsideration Request
This file outlines the process for submitting a reconsideration request to Blue Cross Blue Shield of Nebraska. It is essential for members who need to review processed claims with additional information. Complete the form accurately for a swift response.
Edit, Download, and Sign the BlueCross BlueShield Nebraska Reconsideration Request
Form
eSign
Add Annotation
Share Form
How do I fill this out?
Filling out the reconsideration request form requires careful attention to detail. Begin by providing all necessary member and claim information at the top of the form. Ensure you attach any relevant documentation to support your request.
How to fill out the BlueCross BlueShield Nebraska Reconsideration Request?
1
Enter the member's name and ID number.
2
Provide the BCBSNE claim number and provider details.
3
Indicate the reasons for reconsideration using the applicable boxes.
4
Attach relevant documentation to support your request.
5
Submit the completed form via the preferred submission method.
Who needs the BlueCross BlueShield Nebraska Reconsideration Request?
1
Members who have received a denial on a claim and believe the outcome can change.
2
Providers looking to dispute a reimbursement decision made by BCBSNE.
3
Individuals filing claims for workers' compensation cases needing reconsideration.
4
Patients who need to ensure accurate billing information is reflected in their healthcare records.
5
Insurance coordinators managing benefits that require correction for proper processing.
How PrintFriendly Works
At PrintFriendly.com, you can edit, sign, share, and download the BlueCross BlueShield Nebraska Reconsideration Request along with hundreds of thousands of other documents. Our platform helps you seamlessly edit PDFs and other documents online. You can edit our large library of pre-existing files and upload your own documents. Managing PDFs has never been easier.
Edit your BlueCross BlueShield Nebraska Reconsideration Request online.
Editing the BCBSNE reconsideration request PDF on PrintFriendly is simple and efficient. Utilize our intuitive PDF editor to make necessary changes to the form content. Enhance your document's completeness and accuracy with our editing tools before submission.
Add your legally-binding signature.
Signing the PDF on PrintFriendly is designed to be user-friendly and seamless. Utilize our signature feature to digitally sign the document quickly. Ensure your submission is complete by including your signature alongside your filled form.
Share your form instantly.
Sharing the PDF on PrintFriendly allows for easy collaboration and communication. Use the share feature to send the form directly to relevant parties. Keep all stakeholders informed and involved in the reconsideration process with just a few clicks.
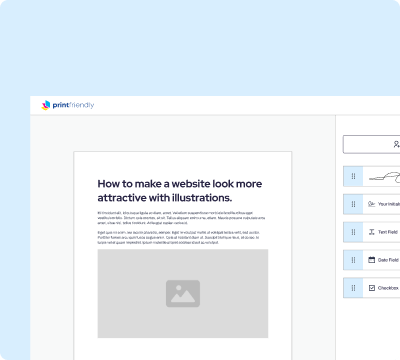
How do I edit the BlueCross BlueShield Nebraska Reconsideration Request online?
Editing the BCBSNE reconsideration request PDF on PrintFriendly is simple and efficient. Utilize our intuitive PDF editor to make necessary changes to the form content. Enhance your document's completeness and accuracy with our editing tools before submission.
1
Upload the BCBSNE reconsideration request PDF to PrintFriendly.
2
Select the text fields you want to edit and input the necessary information.
3
Make any adjustments to formatting as needed for clarity.
4
Save your edited document directly to your device.
5
Print or access the PDF for submission.

What are the instructions for submitting this form?
To submit the reconsideration request form, you can send it via multiple channels. For electronic submission, use NaviNet to upload the completed document directly. Alternatively, you may mail the form to Blue Cross and Blue Shield of Nebraska, Attention: HNR/Reimbursements, PO Box 3248, Omaha NE 68180-0001. If you prefer fax submission, send it to 402-548-4698. Be sure to confirm that all necessary documentation is attached before sending your request.
What are the important dates for this form in 2024 and 2025?
The reconsideration request form is crucial for submitting claims that require review beyond standard processing. In 2024, ensure timely submissions, particularly around peak insurance claims periods. Stay updated on any modifications to requirements or deadlines.

What is the purpose of this form?
The purpose of the reconsideration request form is to provide members and providers a way to formally ask BlueCross BlueShield of Nebraska to review a claim that has been previously processed. This form allows for the inclusion of additional documentation and information that may not have been considered initially. Completing the form accurately and promptly can facilitate the resolution of claim disputes and ensure proper reimbursement.
Tell me about this form and its components and fields line-by-line.
- 1. Member's Name: Enter the name of the member associated with the claim.
- 2. Member's ID Number: Provide the insurance identification number of the member.
- 3. BCBSNE Claim Number: Indicate the claim number assigned by BCBSNE.
- 4. Provider Name: List the name of the healthcare provider.
- 5. Individual NPI: Enter the National Provider Identifier for the individual provider.
- 6. Contact Name: Name of the individual who can be contacted for more information.
- 7. Phone Number: Provide a phone number for communication regarding the claim.
- 8. Patient's Name: Indicate the name of the patient receiving services.
- 9. Relationship: Describe the relationship of the member to the patient.
- 10. Date(s) of Service: The date(s) when the medical services were provided.
- 11. Location of Services: Specify where the services were rendered.
- 12. Clinic Tax ID or NPI: Mandatory identifier for the clinic providing services.
- 13. Address: Mailing address of the member or provider.
- 14. Fax Number: Fax number for sending additional documents, if required.
- 15. Reason for Reconsideration: Checkbox options for selecting the reason for the reconsideration.
- 16. Comments: Space for any additional comments or information relevant to the reconsideration.
What happens if I fail to submit this form?
Failing to submit the reconsideration request form properly can lead to claim denial. It is crucial to provide all requested information to avoid delays. Incomplete submissions may prevent your case from being reviewed.
- Delayed Review: Incomplete forms may result in delays in the reconsideration process.
- Claim Denial: Failure to follow submission guidelines may lead to automatic claim denials.
- Increased Workload: Retrieving and completing forms again increases workload for both the member and provider.
How do I know when to use this form?
- 1. Claim Denial Appeals: Use this form to formally appeal a claim that has been denied.
- 2. Correcting Errors: When errors are identified in processed claims, this form is required to initiate corrections.
- 3. Providing Additional Information: Submit this form if you have new documentation supporting your claim.
Frequently Asked Questions
How do I access the reconsideration request form?
You can download the reconsideration request form directly from our website.
Can I fill out the form electronically?
Yes, you can use our PDF editor to fill out the form electronically.
What should I do if my claim was denied?
Fill out the reconsideration request form and provide additional information for review.
How do I submit the reconsideration request?
You can submit it via mail, fax, or electronically through NaviNet.
Are there any fees for using the reconsideration process?
There are no fees associated with submitting your reconsideration request.
What if I forgot to attach necessary documentation?
Ensure all relevant documents are included to avoid delays in processing your request.
How long does it take to process a reconsideration request?
Processing times may vary, so check with BCBSNE for specific timelines.
Can I track the status of my request?
Yes, use NaviNet to check the status of your reconsideration submission.
What information is required on the form?
All sections, including patient and provider details, must be completed accurately.
Is there a way to expedite the process?
Submitting a well-documented request can help expedite your reconsideration.