Edit, Download, and Sign the BCBSNM Pharmacy Prior Authorization Instructions
Form
eSign
Add Annotation
Share Form
How do I fill this out?
Filling out this form is easy and efficient. Start by ensuring that you have all the necessary patient information on hand. Then, use the electronic link to complete the request accurately.
How to fill out the BCBSNM Pharmacy Prior Authorization Instructions?
1
Gather patient information and verify eligibility.
2
Access the BCBS Pharmacy Prior Authorization link.
3
Fill out the required information in the CoverMyMeds form.
4
Submit the form electronically for processing.
5
Receive immediate confirmation of your submission.
Who needs the BCBSNM Pharmacy Prior Authorization Instructions?
1
Healthcare providers need this file to request prior authorizations for medications.
2
Patients may require confirmation that their prescription is covered under their plan.
3
Pharmacy staff requires access to the form to process prescription requests efficiently.
4
Administrative personnel in healthcare settings need it for documentation and compliance.
5
Insurance companies need this file to determine the eligibility of prior authorization requests.
How PrintFriendly Works
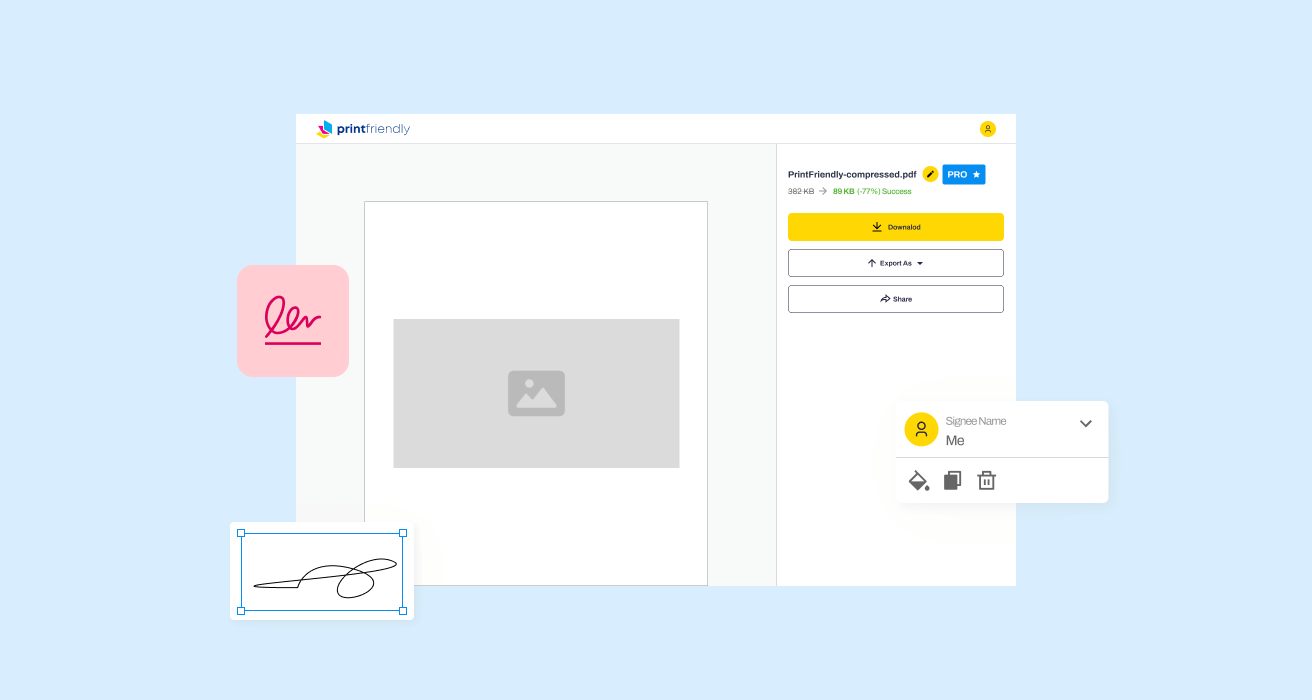
At PrintFriendly.com, you can edit, sign, share, and download the BCBSNM Pharmacy Prior Authorization Instructions along with hundreds of thousands of other documents. Our platform helps you seamlessly edit PDFs and other documents online. You can edit our large library of pre-existing files and upload your own documents. Managing PDFs has never been easier.
Edit your BCBSNM Pharmacy Prior Authorization Instructions online.
You can easily edit this PDF on PrintFriendly by first uploading the document. Once it's uploaded, you can click on any text field to make changes as needed. Save your edits and download the revised document for your records.
Add your legally-binding signature.
Signing the PDF on PrintFriendly is straightforward. You can add your signature by selecting the 'Sign' option and either drawing or uploading your signature. Once signed, you can save and share the document as required.
Share your form instantly.
Sharing the PDF on PrintFriendly is now easier than ever. After editing, simply click the 'Share' button to generate a link. You can copy this link to share with others via email or social media.
How do I edit the BCBSNM Pharmacy Prior Authorization Instructions online?
You can easily edit this PDF on PrintFriendly by first uploading the document. Once it's uploaded, you can click on any text field to make changes as needed. Save your edits and download the revised document for your records.
1
Upload your PDF document to the PrintFriendly platform.
2
Click on any field to edit the text as needed.
3
Make any additional adjustments to the layout and design.
4
Save your changes to ensure all edits are captured.
5
Download the modified PDF to your device for future use.

What are the important dates for this form in 2024 and 2025?
Important dates for the BCBSNM Pharmacy Prior Authorization process will be announced at the beginning of each year. Be sure to stay updated on submission deadlines and changes in policies. Keep an eye on communications from BCBSNM for any potential changes in 2024 and 2025.

What is the purpose of this form?
The primary purpose of this form is to facilitate a streamlined process for prior authorizations in pharmacy settings. It enables healthcare providers to submit requests electronically, ensuring timely approvals and minimizing paperwork. By utilizing this form, providers can enhance their workflow and improve patient care by ensuring necessary medications are accessible swiftly.
Tell me about this form and its components and fields line-by-line.
- 1. Patient Information: Includes patient's name, date of birth, and identifier.
- 2. Medication Details: Specifies the medication name, dosage, and prescribing physician.
- 3. Insurance Information: Captures the insurance provider details along with the member ID.
- 4. Physician Information: Provides details about the prescribing physician including contact information.
- 5. Signature Section: Requires signatures from the patient and the provider for authorization.
What happens if I fail to submit this form?
Failure to submit this form may lead to delays in receiving necessary medications. This can affect patient health and compliance with treatment plans. It is crucial to ensure timely submission to avoid these issues.
- Delayed Treatment: Patients may experience delays in accessing vital medications.
- Increased Workload: Healthcare providers may face increased administrative burden due to resubmissions.
- Insurance Denials: Missing or improperly completed forms may lead to insurance denials.
How do I know when to use this form?
- 1. Prior Authorization Request: To formally request approval for a medication.
- 2. Insurance Verification: To confirm coverage before prescribing a specific drug.
- 3. Compliance Documentation: Used to document the authorization process for audits.
Frequently Asked Questions
How do I access the BCBSNM Pharmacy Prior Authorization form?
You can access the form by navigating to the BCBS Pharmacy Prior Authorization link provided on the Availity portal.
What information do I need to fill out the form?
You will need the patient's details, including their membership information and the specific medication being requested.
Can I edit the PDF after downloading it?
Yes, you can make edits on PrintFriendly before downloading the final version.
Is there a fee to use CoverMyMeds?
No, there is no cost to use CoverMyMeds for submitting prior authorization requests.
How do I know when my request has been processed?
You will receive an immediate confirmation from CoverMyMeds after submission.
What should I do if my request is denied?
If your request is denied, you may contact the pharmacy benefit manager for further clarification or to appeal the decision.
Can multiple requests be submitted at once?
You must submit each request individually to ensure processing accuracy.
What if I forget my CoverMyMeds password?
You can reset your password through the login page on the CoverMyMeds site.
Is there a customer support option if I have questions?
Yes, there is a live chat feature available for support.
How often should I check the status of my request?
Once submitted, you will receive notifications; therefore, you do not need to check the status repeatedly.